Services and solutions
Avenga in numbers
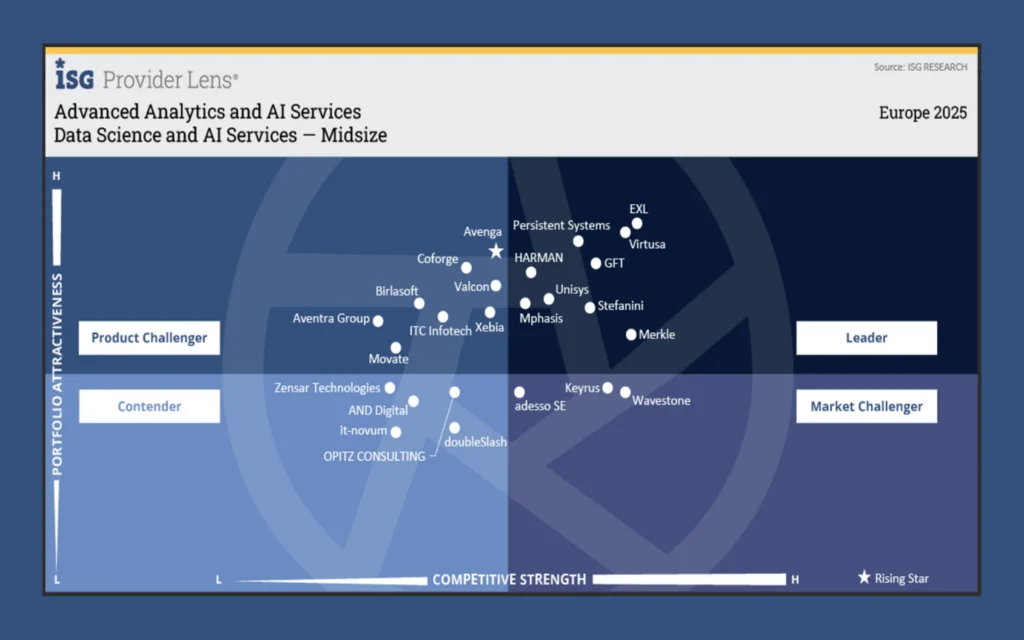
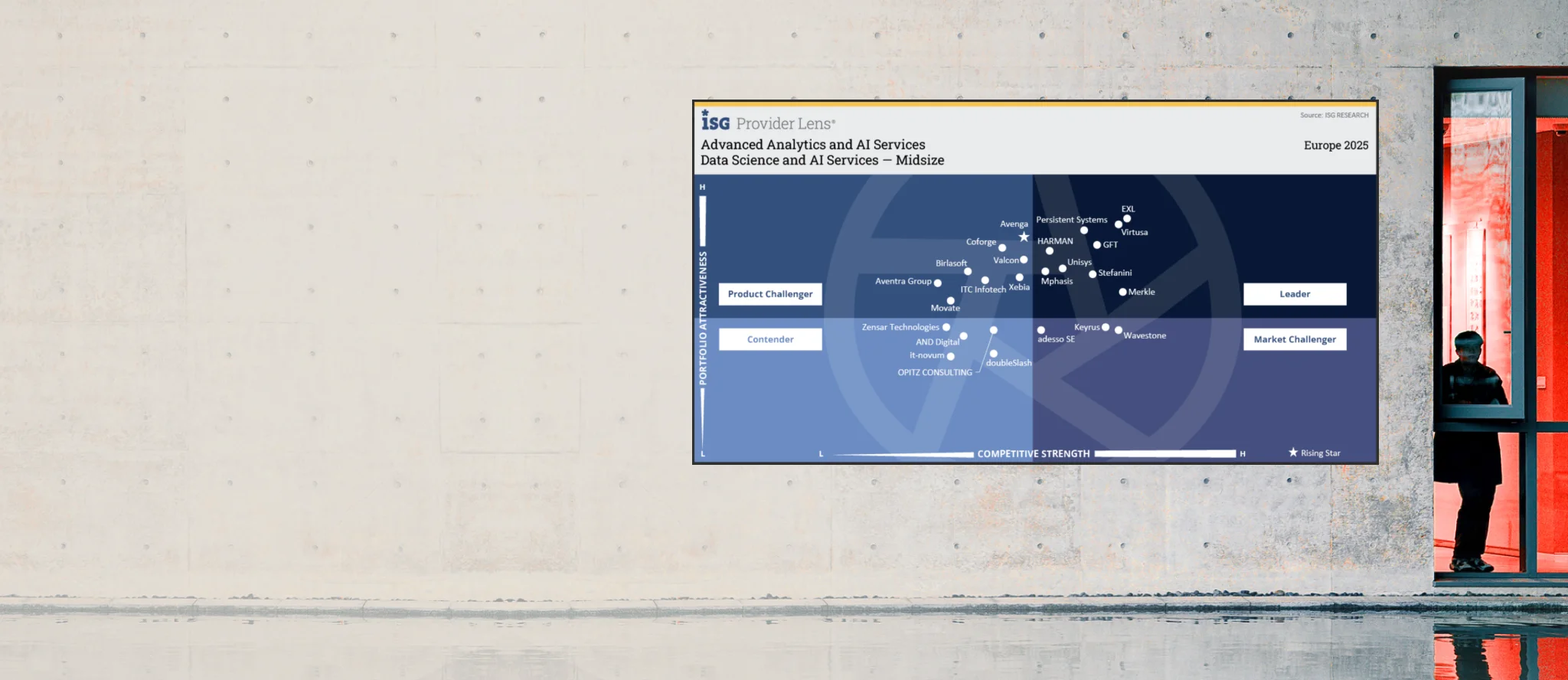
Avenga has been named Europe’s Rising Star for its data and AI capabilities that redefine the market’s perception of customer-centricity in AI development services.
Industries we drive growth in
-
Automotive
Through advanced digital platforms and intelligent systems, we help automotive leaders innovate faster — modernizing engineering, production, and mobility services for safer, cleaner, more adaptive transportation.
Learn more
-
Banking and Financial Services
Empowering financial institutions to reinvent products, operations, and customer experiences, we bring secure digital innovation supported by trusted data intelligence and AI-enhanced decision-making.
Learn more
-
Energy and Utilities
The modernization of energy ecosystems is driven by our innovative digital solutions, enabling resilient infrastructure, smarter resource management, and sustainable growth.
Learn more
-
Life Sciences
By unifying digital platforms, automation, and intelligent insights, we accelerate scientific and commercial innovation, helping organizations bring therapies to market faster and improve patient outcomes.
Learn more
-
Manufacturing
Manufacturers gain sharper quality, agility, and efficiency through our innovation-led approach — powered by connected systems, automation, and predictive intelligence for smarter production.
Learn more
-
Media
Digital platforms that enhance creation, distribution, and audience engagement allow media organizations to innovate at scale, delivering personalized and dynamic experiences.
Learn more
-
iGaming
Innovation within iGaming accelerates through our flexible, secure, and data-driven ecosystems that boost player experience, strengthen integrity, and enable rapid global expansion.
Learn more
-
Mobility
Mobility providers transform operations and user experiences with innovative platforms that connect services, optimize performance, and leverage real-time insights for seamless movement.
Learn more
-
Retail and Consumer
Commerce is reimagined through intelligent, innovative platforms that modernize supply chains, elevate customer relevance, and create frictionless shopping experiences.
Learn more
-
Telecommunications
Telecom operators enhance reliability and scale through our innovation-focused digital architectures, automation, and intelligent optimization — enabling more personalized and resilient connectivity.
Learn more
Proven return on technology investment with Avenga
Elevating logistics risk management with intelligent automation
Slashing review cycles by 86% with automated fraud detection
Sophisticated pharma patient engagement platform

At the heart of everything we do is a passion for solving real-world challenges through technology. Join us and shape the future of industries with us.